Rotator Cuff Tear Arthropathy
- Diagnosis
- Non-operative Options
- Operative Options
- Before Your Surgery
- After Your Surgery
- Your Rehab
What is Rotator Cuff Arthropathy?
The rotator cuff consists of 4 muscles that stabilize the ball and socket joint of the shoulder during movement. Large tears in the rotator cuff can lead to joint instability and slipping of the ball (end of the upper arm bone or humerus) out of the socket (the glenoid fossa of the shoulder). Over time, this leads to a condition called rotator cuff arthropathy, which is a form of wear-and-tear arthritis caused by the rubbing of the ball against the outer rim of the glenoid.
Symptoms of Rotator Cuff Arthropathy
Symptoms of rotator cuff arthropathy include pain, swelling, loss of motion, loss of strength, a sensation of grinding or catching of the joint, shoulder dislocation and muscular atrophy. Overhead activities of daily living such as bathing, dressing and eating become increasingly difficult.
Diagnosis of Rotator Cuff Arthropathy
Diagnosis of a rotator cuff arthropathy will be based on your history and physical examination for restriction in range of motion or muscular atrophy. X-rays may be ordered to evaluate the joint for any bony abnormality or a high riding shoulder, which is a sign of a torn rotator cuff. MRI and CT scans may also be ordered to confirm the diagnosis.
- Physical Therapy Intro
- Shoulder and Elbow Steroid Injection
Non-surgical treatment options include ice, heat, anti-inflammatory medications, steroid injections, and physical therapy with the goal being to preserve range of motion and stability.
Want to know more?
Surgical treatment options may include:
- Arthroscopic debridement: Any damaged soft tissue or bony fragment is removed, and partial repair of the torn rotator cuff may be performed.
- Reverse shoulder replacement surgery: The damaged ball and socket regions of the joint are removed and replaced by artificial components. Instead of replacing with similarly shaped components, the ball-shaped prosthesis is implanted at the glenoid cavity and the cup-shaped prosthesis is implanted at the end of the upper arm bone. This provides better stability and functionality without the need for a rotator cuff.

Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
- After Surgery Video
- Shoulder Surgery Recovery Video
Following surgery, your hand may be placed in a sling.
Want to know more?
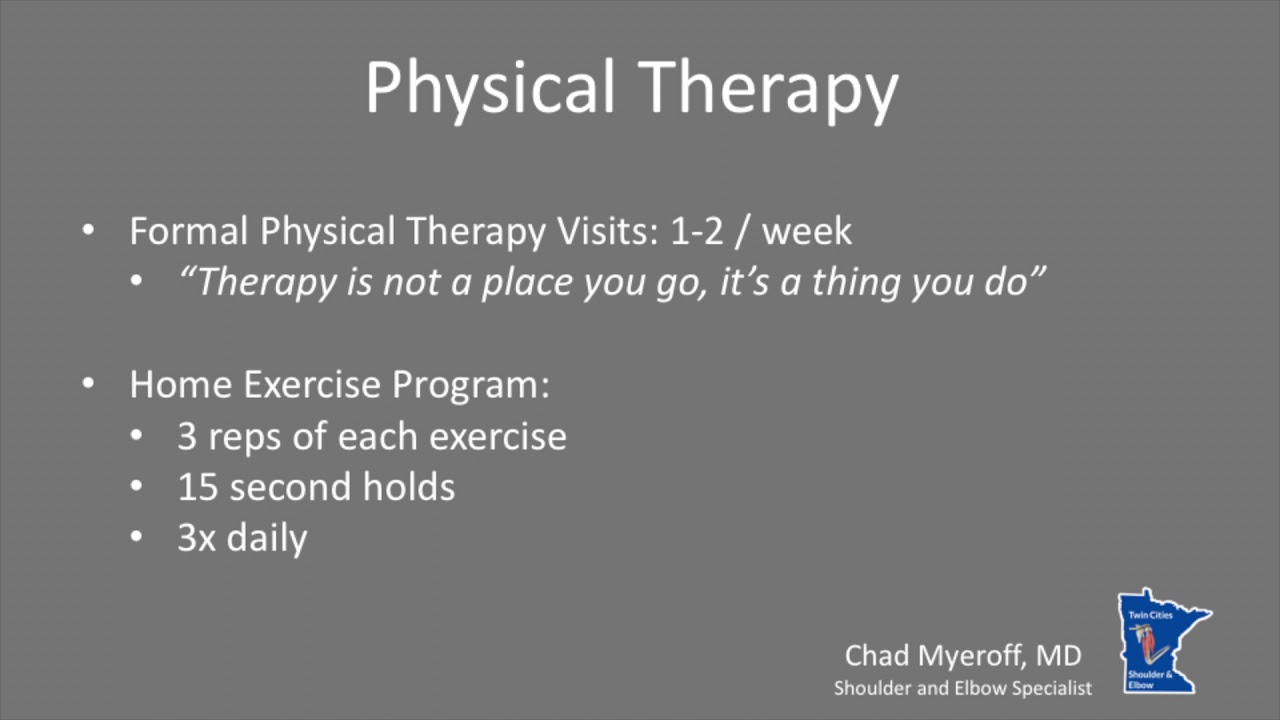
- Physical Therapy Intro Video
- Finger ROM Video
- Standard Elbow ROM Video
- Shoulder ROM Video
Physical therapy rehabilitation may begin the day after surgery to gradually improve your range of motion. Electrical stimulation and massage may also be helpful.