Periprosthetic Fractures
- Diagnosis
- Non-operative Options
- Operative Options
- Before Your Surgery
- After Your Surgery
- Your Rehab
What are Periprosthetic Fractures?
Implants and prostheses inserted into the bones and joints through joint replacement surgery, are helpful in the restoration of function in severely damaged joints. However, over many years, these artificial fixation devices can affect the shape and structure of the bone surrounding it, causing it to weaken and making it susceptible to breakage from even a low-energy fall. This rare condition is termed periprosthetic fracture and is associated with pain, limb-length inequality and deformity.
The goals of management of a periprosthetic fracture are the same as for any fracture, i.e. restoration of the bones in the right position, getting you to walk soon after the procedure, and avoiding complications of disuse such as stiffness and osteoporosis.
X-rays, both past and present, are necessary to evaluate the fracture and implant changes, and classify the fracture based on severity.
Stable periprosthetic fractures may be treated by immobilization with a cast or brace and minimal weight-bearing.
I have specialized interest and training in fractures that occur around total shoulder and total elbow replacements. I have written book chapters on this topic and presented nationally. While some can be managed without surgery, many of these injuries are best treated with surgery to fix the fracture, revise your replacement, or both.
Unstable periprosthetic fractures require surgical intervention. If the implant is firmly attached, an open reduction and internal fixation procedure is carried out by re-aligning the bone fragments and stabilising them using screws and plates. Bone grafts may be used to strengthen the weakened bone. If the implant is loose, your surgeon suggests joint revision surgery, where the implant is removed and replaced by a new prosthesis. Bone grafts may be used to strengthen the weakened bone, and a longer stem is used to secure the prosthesis deeper into the bone.
Complications may arise as a result of poor bone quality (osteoporosis) causing re-fractures, dislocation, limb-length inequality and blood clots.

Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
- After Surgery Video
- Shoulder Surgery Recovery Video
Once you and your doctor decide that surgery will help you, you will need to learn what to expect from the surgery and how to actively participate in the treatment plan for the best results afterward.
Preparing mentally and physically for surgery is an important step toward a successful result. Understanding the process, and your role in it, will help you recover more quickly and have fewer problems.
Before surgery, your doctor will perform a complete physical examination to make sure you don’t have any conditions that could interfere with the surgery or the outcomes.
- Routine tests, such as blood tests and X-rays may be performed.
- Discuss any medications you are taking with your doctor as you may have to stop or alter your intake before surgery. If you are taking aspirin or anti-inflammatory medications or any drugs that increase the risk of bleeding, you will need to stop taking them one week before surgery to minimize bleeding.
- Discuss with your doctor about preparing for potential blood replacement, medical interventions and other treatments prior to surgery.
- Report any infections to your surgeon. Surgery cannot be performed until all infections have cleared up.
- If you smoke, you should stop or cut down as smoking interferes with wound healing and can affect your recovery.
- Have someone available to take you home, as driving is not recommended for at least 24 hours or as advised.
- You may need help with everyday tasks such as cooking, shopping and laundry.
- Put items that you use often within easy reach, so you won’t have to stretch and bend as often.
Want to know more?
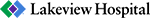
- Physical Therapy Intro Video
- Finger ROM Video
- Standard Elbow ROM Video
- Shoulder ROM Video